老人面对关节退行性变引起的疼痛很普遍,轻则行动不便,重者撑拐杖坐轮椅,生活素质大受影响;近年来,随着手机的刷屏习惯,大量的年轻男女都成了低头族,颈椎退行性变问题(包括富贵包)越来越普及,甚至手指的关节也出现不同程度的劳损退行性变。
关节退行性变导致
一、关节软骨进行性劳损和破坏;二、软骨下骨增厚;三、骨刺形成滑膜炎;四、膝关节韧带和半月板变性;五、关节囊肥大(7,8,9,10,11,12)
主要临床症状
一、慢性疼痛;二、关节不稳;三、关节僵硬;四、关节间隙狭窄(18,19)

成因:
炎症:炎症介质通过MMPs和ADAMTS活性的增加导致软骨ECM降解(13,14,15,16,17)
老化:老化细胞表现出氧化应激增加,从而促进细胞衰老并改变线粒体功能(20,21,22,23)
肥胖:除了增加膝关节的生物力学负荷外,肥胖还被认为通过分泌脂肪组织来源的细胞因子(称为脂肪因子)而导致低级别的全身炎症。(24,25,26)
运动劳动损伤、机械性磨损:
创伤相关的运动损伤可引起骨、软骨、韧带和半月板损伤,所有这些都会对关稳定产生负面影响(26,27,28);软骨组织撕裂、关节脱位、韧带拉伤和撕裂是临床上最常见的可能导致关节炎的损伤(29,30)。
遗传倾向性:
主要通过诱导软骨细胞分解反应来促进关节炎的发展和进展(6);成纤维细胞生长因子(FGF)通路的改变主要通过诱导软骨细胞分解反应来促进关节炎的发展和进展(31,32,33,34,35,36)
当我们面对关节退行性变导致的疼痛,目前在药物上面的治疗,广泛使用的是氨基葡萄糖,但治疗效果差强人意。关于氨基葡萄糖的问题,国际上也有了更新的研究,这个研究成果我们以后再专门介绍。我们现在有更安全更理想的修补方案可选择。
今天就跟大家探讨一下德国最新的一些与关节退行性变有关的新临床研究。先探讨关节退行性变导致的疼痛或者行动不便,甚至坐轮椅撑拐杖;以后还会与大家探讨别的关节问题,包括痛的要命的痛风、还有类风湿性关节炎、强直性脊椎炎等等。希望大家多加留意或者关注我们。
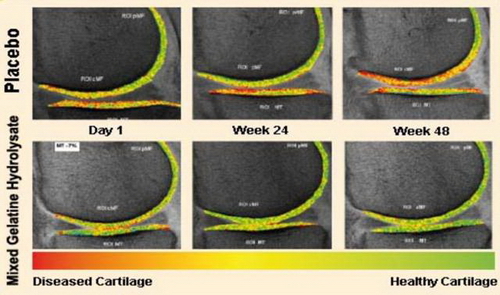
早于2000年时,克利夫兰大学医院的Moskowitz RW博士等人已进行了胶原水解物在骨关节疾病中的作用(2,37);2016和2017 M Schunck 及S Oesser两位学者在德国的研究发现,用新鲜牛皮提炼的<水解骨胶原蛋白>可以修复关节软组织,促进软骨的再生。水解骨胶原蛋白是胶原蛋白的水解产物,与关节软骨中主要成分2型的胶原蛋白相似(3)。与大分子的胶原相比,水解产物更容易被人体吸收,用来修补因关节退行性变而导致的关节软骨的流失,同时减少关节的疼痛(1,5)。
此外,德国弗赖堡大学施瓦兹沃德斯特尔分校的Daniel KönigSteffen Oesser, Stephan Scharla, Denise Zdzieblik及 Albert Gollhofer 等学者在2018年的另一项研究,发现每天口服5克的水解骨胶原蛋白,可以增加停经后妇女腰椎和股骨颈的密度,大大缓解因矿物元素流失而引起的骨质疏松症的风险(4)。
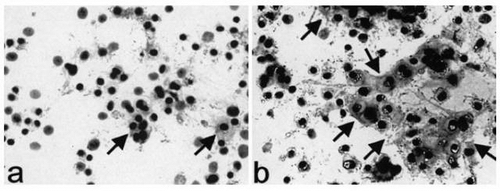
水解骨胶原蛋白也可以刺激韧带细胞外基质的生物合成,在2013年的研究发现,水解骨胶原蛋白可以增加50%弹性蛋白生物的合成,同时增加了2.4倍的胶原蛋白的合成,在预防韧带和肌腱病理性的病变起到了积极的作用(3)。
除了针对软组织的修补外,医学界同时还要面对其它关节退行性变的挑战;怎样解决关节内粘连(Intraarticular adhesion)(38)、纤维化(fibrosis)(39)、软骨钙化(cartilage calcification) (40)(骨刺-骨质增生)问题。因要解决骨关节整体退行性变问题,修补软组织只完成小部份任务;发炎、粘连、纤维化、软骨钙化也需要别的研究突破来处理的,所以我们必须从生物医学、营养医学等各方面,全面去研究。 希望国内相关大学、医学院、科研机构也能投入更多资源、精力在相关领域的临床研究,能够超越欧美成就,带领医学进入新阶段! 下次再跟大家分享更多国际上的新研究;如痛风、强直性脊椎炎、类风湿性关节炎等等。有兴趣了解更多关节研究话题的,欢迎关注我们。
身边如果有任何人正在面对关节疼痛的问题,欢迎大家把这一篇内容转发给他们。希望这些学术研究成果能为他们带来新的希望,为他们带来更理想的治疗方案。
本文章属於拜塞复康中心团队原创,如要转载请联同作者机构一并转发,否则需取得作者书面同意方能节录引用。
医学文章需要专业、认真、严谨的态度,您的转发和点赞会成为我们的重大动力,谢谢。
原创:拜塞复康中心
张阳生(顾问医生)、高建伟(顾问医生)
欧阳宏基(香港脊骨神经科医生)、
马圆(英国注册营养师)、施丹虹(香港营养学家)
郑志雄(加拿大放射影像物理学家)
了解更多
参考文献:
1.Bakilan F, et al. (2016) “Effects of Native Type II Collagen Treatment on Knee Osteoarthritis: A Randomized Controlled Trial.” The Eurasian Journal of Medicine. 48(2): 95-101
2.Moskowitz RW et al. Role of collagen hydrolysate in bone and joint disease. Seminars in arthritis and rheumatism Vol 30, No 2 (Oct) 2000 pp87-99.
3.Schunk M, et al. (2013) “Specific collagen peptides benefit the biosynthesis of matrix molecules of tendons and ligament.” Journal of the international Society of Sports Nutrition. 10(1):23
4.Oesser S, et al. (2018) “Specific Collagen Peptides Improve Bone Mineral Density and Bone Markers in Postmenopausal Women—A Randomized Controlled Study.” Nutrients. 10(1):97.
5.Oesser S, et al. (2017) “Improvement of activity-related knee joint discomfort following supplementation of specific collagen peptides.” Applied Physiology, Nutrition, and Metabolism. 42: 588–595
6.Modulating hedgehog signaling can attenuate the severity of osteoarthritis.Lin AC, Seeto BL, Bartoszko JM, Khoury MA, Whetstone H, Ho L, Hsu C, Ali SA, Alman BA Nat Med. 2009 Dec; 15(12):1421-5.
7.Osteoarthritis: a disease of the joint as an organ.Loeser RF, Goldring SR, Scanzello CR, Goldring MB Arthritis Rheum. 2012 Jun; 64(6):1697-707.
8.Loeser RF, Goldring SR, Scanzello CR et al. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum 2012; 64: 1697–1707.
9.Felson DT. Clinical practice. Osteoarthritis of the knee. N Engl J Med 2006; 354: 841–848.
10.Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol 2007; 213: 626–634.
11.Krasnokutsky S, Samuels J, Abramson SB. Osteoarthritis in 2007. Bull NYU Hosp Jt Dis 2007; 65: 222–228.
12.Loeser RF. Aging and osteoarthritis: the role of chondrocyte senescence and aging changes in the cartilage matrix. Osteoarthritis Cartilage 2009; 17: 971–979.
13.Kim JH, Jeon J, Shin M et al. Regulation of the catabolic cascade in osteoarthritis by the zinc-ZIP8-MTF1 axis. Cell 2014; 156: 730–743.
14.Hirata M, Kugimiya F, Fukai A et al. C/EBPbeta and RUNX2 cooperate to degrade cartilage with MMP-13 as the target and HIF-2alpha as the inducer in chondrocytes. Hum Mol Genet 2012; 21: 1111–1123.
15.Little CB, Barai A, Burkhardt D et al. Matrix metalloproteinase 13-deficient mice are resistant to osteoarthritic cartilage erosion but not chondrocyte hypertrophy or osteophyte development. Arthritis Rheum 2009; 60: 3723–3733.
16.Glasson SS, Askew R, Sheppard B et al. Deletion of active ADAMTS5 prevents cartilage degradation in a murine model of osteoarthritis. Nature 2005; 434: 644–648.
17.Barnholtz-Sloan JS, Severson RK, Stanton B et al. Pediatric brain tumors in non-Hispanics, Hispanics, African Americans and Asians: differences in survival after diagnosis. Cancer Causes Control 2005; 16: 587–592.
18.Clinical practice. Osteoarthritis of the knee. Felson DT N Engl J Med. 2006 Feb 23; 354(8):841-8.
19.Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F, National Arthritis Data Workgroup. Arthritis Rheum. 2008 Jan; 58(1):26-35.
20.Loeser RF. Aging and osteoarthritis. Curr Opin Rheumatol 2011; 23: 492–496.
21.Kim J, Xu M, Xo R et al. Mitochondrial DNA damage is involved in apoptosis caused by pro-inflammatory cytokines in human OA chondrocytes. Osteoarthritis Cartilage 2010; 18: 424–432.
22.Goodwin W, McCabe D, Sauter E et al. Rotenone prevents impact-induced chondrocyte death. J Orthop Res 2010; 28: 1057–1063.
23.Naik E, Dixit VM. Mitochondrial reactive oxygen species drive proinflammatory cytokine production. J Exp Med 2011; 208: 417–420.
24.Conde J, Scotece M, Gomez R et al. Adipokines and osteoarthritis: novel molecules involved in the pathogenesis and progression of disease. Arthritis 2011; 2011: 203901.
25.Das UN. Is obesity an inflammatory condition? Nutrition 2001; 17: 953–966. Fain JN. Release of inflammatory mediators by human adipose tissue is enhanced in obesity and primarily by the nonfat cells: a review. Mediators Inflamm 2010; 2010: 513948.
26.Radin EL. Who gets osteoarthritis and why? J Rheumatol Suppl, 2004; 70: 10–15.
27.Andriacchi TP, Mundermann A, Smith RL et al. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng 2004; 32: 447–457.
28.Miyazaki T, Wada M, Kawahara H et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis 2002; 61: 617–622.
29.Fridén T, Sommerlath K, Egund N et al. Instability after anterior cruciate ligament rupture. Measurements of sagittal laxity compared in 11 cases. Acta Orthop Scand 1992; 63: 593–598. Sernert N, Kartus JT Jr, Ejerhed L et al. Right and left knee laxity measurements: a prospective study of patients with anterior cruciate ligament injuries and normal control subjects. Arthroscopy 2004; 20: 564–571.
30.Modulating hedgehog signaling can attenuate the severity of osteoarthritis. Lin AC, Seeto BL, Bartoszko JM, Khoury MA, Whetstone H, Ho L, Hsu C, Ali SA, Alman BA Nat Med. 2009 Dec; 15(12):1421-5.
31.Serra R, Johnson M, Filvaroff EH et al. Expression of a truncated, kinase-defective TGF-beta type II receptor in mouse skeletal tissue promotes terminal chondrocyte differentiation and osteoarthritis. J Cell Biol 1997; 139: 541–552.
32.Shen J, Li J, Wang B et al. Deletion of the transforming growth factor beta receptor type II gene in articular chondrocytes leads to a progressive osteoarthritis-like phenotype in mice. Arthritis Rheum 2013; 65: 3107–3119.
33.Wang M, Tang D, Shu B et al. Conditional activation of beta-catenin signaling in mice leads to severe defects in intervertebral disc tissue. Arthritis Rheum 2012; 64: 2611–2623.
34.Mirando AJ, Liu Z, Moore T et al. RBP-Jkappa-dependent Notch signaling is required for murine articular cartilage and joint maintenance. Arthritis Rheum 2013; 65: 2623–2633.
35.Lories RJ, Corr M, Lane NE. To Wnt or not to Wnt: the bone and joint health dilemma. Nat Rev Rheumatol 2013; 9: 328–339.
36.Sassi N, Laadhar L, Allouche M et al. WNT signaling and chondrocytes: from cell fate determination to osteoarthritis physiopathology. J Recept Signal Transduct Res 2014; 34: 73–80.
37.From the Case Western Reserve University; Division of Rheumatic Diseases, University Hospitals of Cleveland, OH. Roland W. Moskowitz, MD: Professor of Medicine, Case Western Reserve University; Director, Division of Rheumatic Diseases, University Hospitals of Cleveland Dr. Moskowitz was the Principal Investigator and Con-sultant for a study on pharmaceutical collagen hydrolysate for DGF Stoess. doi:10.1053/sarh.2000.9622
38.Osteoarthritic cartilage fibrillation is associated with a decrease in chondrocyte adhesion to fibronectin By Muriel Piperno,Pascal Reboul†, Marie-Pierre Hellio le Graverand,Mj Peschard †,Marliese Annefeld‡, M. Richard† and Eric Vignon Claude Bernard University. Centre Hospitalier Lyon Sud, 165 chemin du Grand Revoyet, 69495 Pierre Be ?nite; †Department of Biochemistry, INSERM-CNRS U189, Lyon Sud Medical School, BP 12, 6992
39.Treatment and Rehabilitation of Arthrofibrosis of the KneeScott E. Lawrance MS, PT, ATC, CSCS, K. Donald Shelbourne MD, in Clinical Orthopaedic Rehabilitation: a Team Approach (Fourth Edition), 2018
40.CALCIFICATION OF HUMAN ARTICULAR KNEE CARTILAGE IS PRIMARILY AN EFFECT OF AGING RATHER THAN OSTEOARTHRITIS. H Mitsuyama,* RM Healey,* RA Terkeltaub,# RD Coutts,* and D Amiel*


